Step-by-Step Guide to Becoming a Healthcare Project Manager (2026-27)
Becoming a healthcare project manager in 2026 to 2027 is not about memorizing job descriptions. It is about learning how hospitals, payers, clinics, and vendors actually make decisions, then proving you can deliver change safely, fast, and under constraints.
This guide gives you a practical path, the skills to build, the projects to target, and the proof employers look for, so you can move from interested to hireable with a real portfolio and a credible story.
1) What a Healthcare Project Manager Really Does in 2026 to 2027
Healthcare project management is delivery under high stakes. Timelines matter, but so do patient safety, privacy, regulatory risk, clinical adoption, and operational continuity. In 2026 to 2027, the role is expanding because healthcare systems are under pressure to modernize without breaking care delivery. Digital transformation work keeps accelerating inside PMOs, which is why the mindset in digital transformation across PMOs matters even more in hospitals and health networks.
A healthcare project manager typically runs projects like EHR optimization, scheduling and capacity initiatives, revenue cycle improvements, new clinic rollouts, cybersecurity remediation, AI workflow pilots, supply chain redesign, and quality compliance programs. Those initiatives look like standard projects on paper, but the hidden complexity is clinical adoption, multi stakeholder governance, and audit readiness. If you already understand the PMO ladder from a big picture view, borrow the structure from the chief project officer roadmap and scale it down into a healthcare focused delivery story. You will be judged less on theory and more on whether you can manage complexity with calm, evidence, and decision quality.
The demand side is also real. Economic pressure is changing budgets, staffing models, and procurement patterns, so projects are being prioritized for ROI and resilience. Read the signals in global inflation’s impact on project budgets and translate it into healthcare reality: leaders want projects that reduce waste, shorten cycle times, improve throughput, and protect reimbursement. That is why the best healthcare PMs can speak operations and finance, not just tasks.
You also need to understand how methodologies are evolving. Agile demand is rising across industries, but in healthcare it often becomes hybrid delivery with more governance checkpoints. Use the macro context from rising demand for agile project management and the market framing in economic uncertainty increasing agile demand to position yourself as someone who can choose the right approach, not someone who worships a framework.
Finally, healthcare has a specific career advantage: your projects naturally touch compliance, risk, and security. If you can show that you understand why major cybersecurity concerns prompt PM software overhaul and how that connects to healthcare privacy and patient safety, you will stand out immediately.
2) Step 1: Learn the Healthcare Domain Without Getting Lost
Most aspiring healthcare PMs fail because they learn random facts instead of building a decision model. Your goal is to understand how care is delivered, how money flows, and where risk lives. Start by splitting the ecosystem into four arenas: clinical operations, revenue cycle, IT and data, and governance. You do not need a medical degree, but you do need to understand where clinical time is scarce and why adoption friction is brutal. That friction is the same reason many organizations invest in better tooling and processes, as seen in investment in PM software surging.
Clinical operations means patient access, scheduling, triage, inpatient throughput, discharge planning, and staff workflows. Revenue cycle means eligibility, coding, claims, denials, and reimbursement timing. IT and data means EHR workflows, integrations, reporting, identity access, and security. Governance means approvals, committees, procurement, risk reviews, and compliance. When you can explain how a project touches all four arenas, you sound like someone who can actually run healthcare change, not someone who can only manage tasks.
Pick a realistic project type and study it deeply. If you choose scheduling optimization, your KPIs are no show rate, time to third next available appointment, provider utilization, and patient satisfaction. If you choose denial reduction, your KPIs are denial rate, days in AR, clean claim rate, and appeal cycle time. If you choose a cybersecurity program, your KPIs are remediation velocity, control coverage, and incident risk reduction, which connects naturally to the industry pressure described in major cybersecurity concerns.
Then build a healthcare vocabulary that is operational, not academic. Learn what a super user is, what hypercare means, why downtime procedures exist, and how clinical champions drive adoption. Healthcare teams respect PMs who protect staff time and reduce change fatigue. Your job is to make change feel safe and structured. This is the same leadership posture you see at higher levels in the project portfolio manager guide, just applied to frontline realities.
Finally, get fluent in constraints. Projects are not delayed because PMs lack motivation. They are delayed because clinicians have shifts, committees meet monthly, vendors miss deliverables, and training windows are narrow. You will stand out if you can plan around constraints and still deliver. That is why modern PMOs are leaning into better planning and execution maturity, a theme across digital transformation and AI adoption in project management.
3) Step 2: Build the PM Skill Stack That Healthcare Hiring Managers Trust
Healthcare hiring managers want evidence of structure. They do not want theory. Build your stack in layers: foundations, delivery systems, and proof.
Foundations are scope, schedule, risk, and communication. This is where a credential can accelerate trust, especially if you have limited experience. If you want the fastest credibility boost, follow the study approach in the ultimate PMP exam guide and pressure test yourself with the logic in top PMP exam questions. If you are earlier career, use the structure in the CAPM passing guide and align your positioning with CAPM salary and career insights.
Delivery systems are how you run the work week to week. In healthcare, you need a system that supports governance, clinical adoption, and audit trails. Use weekly status updates that highlight decisions needed, risks, and constraints. Use a decision log so nobody rewrites history later. Use a cutover checklist with rollback steps. Use hypercare staffing plans. These artifacts are more valuable than buzzwords, and they are exactly what differentiates a PM who can deliver from a PM who only coordinates meetings.
Methodology is where many candidates get trapped. Hiring managers are not selecting you because you worship agile. They are selecting you because you can choose a delivery model that fits risk. Learn agile principles because they help with prioritization and feedback loops. Then learn how to operate hybrid delivery with governance checkpoints because that is common in hospitals. That strategic flexibility becomes easier to defend when you reference broader market patterns like rising demand for agile and the business pressure context in economic uncertainty and agile demand.
If your market values PRINCE2, build that option too. PRINCE2 language often matches governance heavy environments. Use the PRINCE2 exam guide, then sharpen decision making with PRINCE2 top questions and the selection logic in PRINCE2 Foundation vs Practitioner. Pair that with a timeline like the four week PRINCE2 study plan so your learning is disciplined.
Proof is the final layer. Healthcare employers love measurable outcomes and clean artifacts. Build three mini case studies even if you are not employed in healthcare yet: a scheduling access improvement, a denial reduction project, and an EHR workflow optimization pilot. Each case study should include the problem, the baseline, the plan, stakeholder map, risks, and a measurable outcome. You can simulate data responsibly by stating assumptions, but the structure must be real. This is the same portfolio mindset that helps people win in freelance project management careers and when starting a project management consultancy firm.
4) Step 3: Get Experience Fast With a Portfolio That Hiring Managers Believe
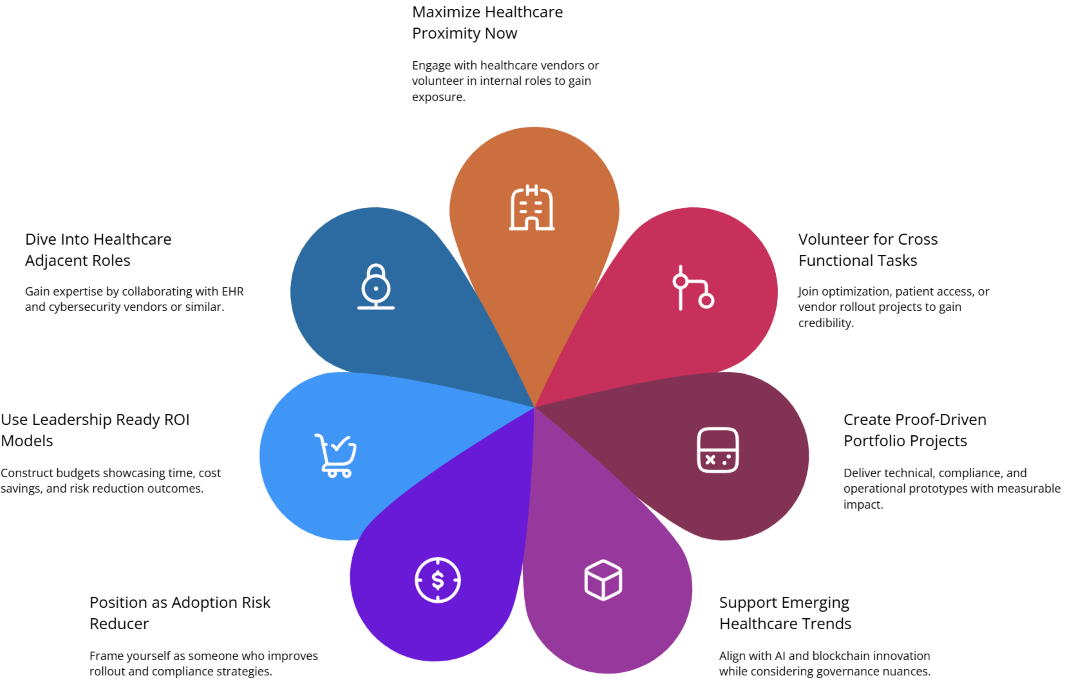
You can break into healthcare PM work without waiting for someone to give you permission. The fastest route is to build credible proof through proximity, projects, and positioning.
Proximity means getting close to healthcare work environments. If you are already inside healthcare in any role, volunteer for cross functional initiatives. Offer to support an EHR optimization, a patient access improvement, a documentation cleanup, or a vendor rollout. If you are outside healthcare, target healthcare adjacent vendors: EHR vendors, revenue cycle platforms, staffing platforms, telehealth vendors, and cybersecurity vendors selling into healthcare. Vendor side roles often give you exposure to healthcare workflows and stakeholders, which transfers well.
Projects means doing work that looks like real delivery. Build three portfolio projects with artifacts. One should be operational, one should be technical, and one should be risk or compliance focused. For technical projects, connect your narrative to the direction of the market such as AI adoption in PM and practical implementation stories like blockchain momentum in PM, not because you will deploy blockchain in a hospital tomorrow, but because it shows you understand emerging tooling and governance tradeoffs.
For operational projects, learn how to create benefits cases that leadership trusts. This is where the budgeting context from global inflation’s impact becomes practical: you must show cost savings, time savings, risk reduction, or revenue protection. Use a simple ROI model, document assumptions, and define how you would measure outcomes after launch. Employers want PMs who can defend value, not just deliver outputs.
Positioning means learning how to speak like a healthcare PM. Stop saying you are organized. Everyone says that. Instead, say you reduce adoption risk by building clinician champion networks, you reduce go live risk by planning rollback and hypercare, and you reduce compliance risk by designing audit ready documentation. These statements are believable only if you can show artifacts, which is why your portfolio matters more than your title.
If you want extra leverage, widen your scope across geographies and work modes. Many healthcare organizations now use remote delivery for IT and transformation programs. Use the tactics in the remote and virtual PM roles guide to build credibility in distributed collaboration, executive reporting, and structured decision logs. That makes you hireable beyond your local market.
Finally, consider global exposure. Healthcare systems vary, but the PM skills transfer. If you can frame your work through international governance and multi cultural stakeholders, the narrative in the international project manager guide gives you language to describe that complexity without sounding vague.
5) Step 4: Win the Job With Targeting, Interview Control, and a 90 Day Plan
Healthcare PM job searches are won by focus. Do not apply to 200 roles with a generic resume. Choose a lane: clinical ops transformation, revenue cycle projects, health IT implementation, cybersecurity programs, or digital transformation PMO work. Then tailor your story and artifacts to that lane.
Start with targeting. If you want higher volume opportunities, aim for large healthcare markets and systems. Use regional market guides to decide where the opportunity density is highest. For example, study your compensation and employer landscape through project management careers in California, New York project management career guide, project management careers in Texas, and Florida project management job market. If you want city level targeting, use project management in New York City, Los Angeles opportunities, Chicago salary analysis, and Dallas Fort Worth insights.
Next, build a resume that reads like proof. Your bullets should show baseline, action, and measurable outcome. Even if your outcomes are small, they must be real. Replace vague words like supported or assisted with delivered, reduced, accelerated, standardized, and prevented, but only when you can defend it. Add a portfolio link with three case studies and downloadable artifacts.
In interviews, control the frame. Most candidates answer questions. Strong candidates lead with a delivery narrative. Use a simple structure: project context, stakes, stakeholders, plan, risks, decisions, outcome, lessons. Then anchor your readiness with a 90 day plan. Your 90 day plan should include stakeholder mapping, workflow discovery, KPI baselining, governance cadence, risk library creation, and a quick win project that reduces pain fast. That is how you build trust.
Also prepare for methodology questions. If asked agile vs waterfall, do not argue ideology. Say you select the delivery approach based on risk, governance, and adoption, using hybrid where needed. The industry context from agile demand supports your story, but your real credibility is how you describe tradeoffs and risk mitigation.
If you want to negotiate better, position yourself as a PM who reduces risk and accelerates measurable outcomes. Leaders pay more for that. And if you want a longer term career ladder, study how PMs grow into portfolio and executive roles using the trajectory described in the project portfolio manager guide and the broader leadership narrative in the chief project officer roadmap.
6) FAQs: Becoming a Healthcare Project Manager in 2026 to 2027
-
You need evidence you can deliver structured change under constraints. A healthcare background helps, but it is not mandatory if you can show domain understanding and credible artifacts. Build a portfolio that includes stakeholder mapping, a risk register, a project plan, and measurable KPIs tied to healthcare outcomes like access, throughput, or reimbursement. Pair that with a recognized PM credential path. If you are early career, the structure in the CAPM guide can help you formalize fundamentals. If you are mid career, a PMP aligned narrative using the PMP exam guide positions you for larger healthcare programs.
-
Target projects with clear KPIs and visible stakeholder groups. Scheduling access improvements, denial reduction initiatives, EHR workflow optimization, clinic rollout standardization, and cybersecurity remediation are strong entry points because the impact is measurable and leaders care. Choose one operational project and one technical project so your portfolio shows range. If you want to position for remote programs, align with delivery skills in the remote and virtual PM roles guide so employers see you can manage cross functional teams without chaos.
-
Not always, but it is a strong trust accelerator, especially in large systems with mature PMOs. Many hiring managers use credentials as a filter when applicant volume is high. If you want to pursue it, use the strategy in the ultimate PMP guide and sharpen decision logic with PMP exam questions. If you are earlier stage, CAPM can be a stepping stone with a clearer entry path, plus it pairs well with a strong portfolio.
-
Prove it through decision quality. Build a case study with a realistic workflow map, stakeholder map, risk register, governance cadence, and benefits plan. Use publicly known healthcare constraints like clinical time limits, training windows, downtime procedures, and vendor dependencies. Then show how you would run discovery, protect staff time, and measure outcomes after launch. Tie your story to macro PMO trends such as digital transformation across PMOs and the operational pressure in global inflation’s impact on budgets to demonstrate you understand why healthcare leaders prioritize certain projects.
-
Stop applying broadly and start targeting a lane. Pick one healthcare project category, tailor your resume to outcomes in that lane, and attach a portfolio with three case studies. Use a simple 90 day plan in interviews to show how you will create clarity and momentum. Also consider adjacent entry points: vendors selling into healthcare, payer operations, and consulting projects. If you want to expand your opportunity pool geographically, use market guides like California PM careers or New York City PM careers to target regions with higher project density.
-
Your first 30 days should be about clarity and risk reduction. Build stakeholder maps for each workstream, baseline KPIs, define a governance cadence, and create a risk library with owners. Capture current workflows before proposing changes. Identify one quick win that reduces daily friction for staff, such as a form simplification, a handoff fix, or a reporting cleanup. Set expectations on hypercare and training early. This approach mirrors what high maturity PMOs do in broader contexts like investment in PM software and agile demand trends, but applied to healthcare realities.
-
Yes, especially in health IT, transformation, vendor implementations, analytics, and PMO roles where delivery is cross functional and meeting driven. The key is proving you can run cadence, manage dependencies, and drive decisions without being onsite. Build artifacts that show structured governance and clear reporting. Then use the positioning tactics from the remote and virtual project management guide so your narrative is credible. Remote roles still require strong stakeholder management, especially when clinical teams are under time pressure.