Best Project Management Software for Healthcare Projects
Project management in healthcare isn’t about hitting deadlines—it’s about saving lives, maintaining compliance, and protecting sensitive data. Unlike standard industries, healthcare organizations must balance clinical safety protocols, HIPAA compliance, and cross-functional team coordination while managing hundreds of interdependent workflows. A missed handoff or a scheduling error isn’t just an inconvenience—it’s a risk to patient outcomes, revenue cycles, and regulatory standing. That’s why choosing the right project management software for healthcare is no longer a matter of convenience; it’s a strategic decision that directly impacts operational integrity.
The healthcare sector is now flooded with PM tools, but very few can handle the intense regulatory needs, constant audits, and complex multi-stakeholder workflows required in clinical and hospital environments. From EHR integration and care coordination to biotech trial tracking, the right software must offer more than Gantt charts. This guide will break down the unique demands of healthcare project management, compare top tools built for these environments, and help you confidently select and implement the right solution.
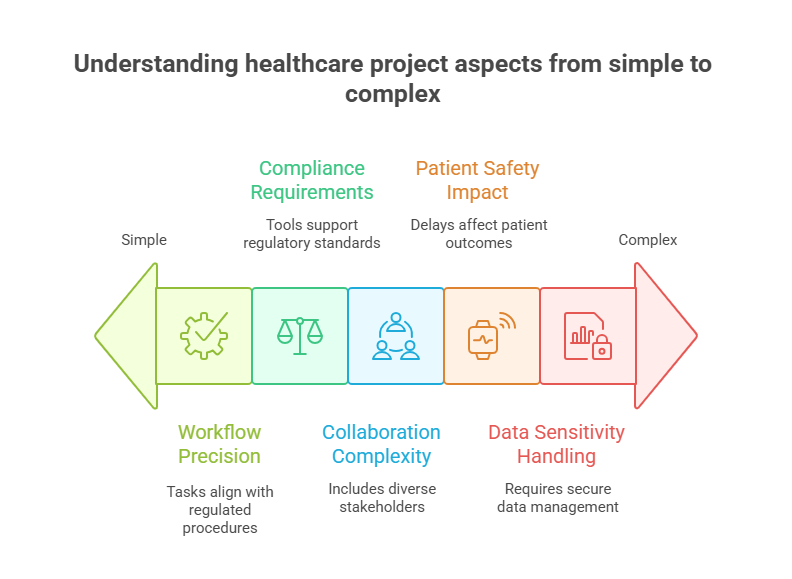
Unique PM Needs in Healthcare Settings
Project management in healthcare operates within a high-stakes, high-regulation ecosystem. Unlike general industries where flexibility can be tolerated, healthcare workflows require precision, accountability, and traceability across every task. These demands shape the way software must function—from real-time updates to role-based access control and audit trails.
Clinical Timelines, Compliance, Cross-Team Collaboration
Clinical projects, whether hospital-based or research-driven, rely on strict timeline enforcement. Delays in one department can cascade into critical disruptions—especially in patient onboarding, surgical coordination, or trial milestones. Project managers must maintain clear dependencies, deadline monitoring, and escalation paths.
Compliance adds another layer. Healthcare teams must adhere to standards like HIPAA, FDA 21 CFR Part 11, and The Joint Commission’s protocols, often simultaneously. Traditional PM tools don’t provide regulatory documentation features like signature validation, secure time-stamping, or compliance logs.
Lastly, collaboration isn’t confined to internal teams. Projects often involve clinicians, IT staff, procurement officers, vendors, insurers, and regulatory bodies. A PM tool in healthcare must facilitate asynchronous communication, centralized task tracking, and transparency across roles—without sacrificing data privacy.
Patient Safety & Data Sensitivity
Patient safety is the non-negotiable cornerstone of every healthcare project. Whether implementing new treatment pathways or coordinating EMR transitions, poor project oversight can introduce safety gaps. A project manager must proactively identify bottlenecks that affect patient flow, clinical task delays, or redundant procedures that can compromise care.
Equally important is the handling of sensitive data. Medical records, clinical results, and billing data must be protected under multiple laws. A healthcare project management system must support role-based permissions, end-to-end encryption, and secure mobile access for remote clinical teams. Any breach or misstep can lead to patient harm and steep penalties.
What sets healthcare PM apart is that failures aren’t just logistical—they’re clinical. Every checklist missed or follow-up delayed could result in preventable outcomes. That’s why any software being considered must have built-in risk mitigation features like escalation triggers, real-time dashboards, and incident response timelines tailored to the healthcare lifecycle.
Top Software Options Compared
Healthcare organizations require project management platforms that balance task precision, HIPAA compliance, and interdisciplinary coordination. Below is a breakdown of four top contenders—Asana, Smartsheet, ClickUp, and Monday.com—evaluated specifically for healthcare relevance. While many tools are adaptable, only a few can deliver secure, scalable, healthcare-ready environments.
Asana, Smartsheet, ClickUp, Monday (Feature Overview)
Each of these tools has seen growing adoption across hospitals, health systems, CROs, and public health departments. But their suitability varies depending on scale, specialty, and internal processes.
Key Factors for Healthcare Use:
HIPAA-readiness or ability to integrate via compliant frameworks
Automation capabilities for repetitive clinical or admin workflows
Template availability for care coordination, credentialing, onboarding
Reporting and audit trail features built for compliance teams
Flexibility in user roles and permission levels to avoid data overexposure
Below is a side-by-side comparison of features:
| Provider | Healthcare Templates | HIPAA Support | Customization & Automation | Best For |
|---|---|---|---|---|
| Asana | Limited (third-party integrations available) | Not HIPAA-compliant by default | High – supports rules, custom workflows | Large-scale admin projects and vendor management |
| Smartsheet | Moderate (clinical trial, IT operations templates) | HIPAA available under Enterprise plan | Very High – dashboards, custom formulas, reports | Clinical research tracking and complex IT rollouts |
| ClickUp | Extensive (EHR workflows, compliance logs, care plans) | Available on Business Plus and Enterprise plans | Extremely High – nested tasks, roles, automation | Cross-functional teams in hospitals or large clinics |
| Monday.com | Basic (customizable with health-focused add-ons) | HIPAA on Enterprise plan only | Moderate – visual workflows, drag-and-drop logic | Smaller providers needing intuitive task coordination |
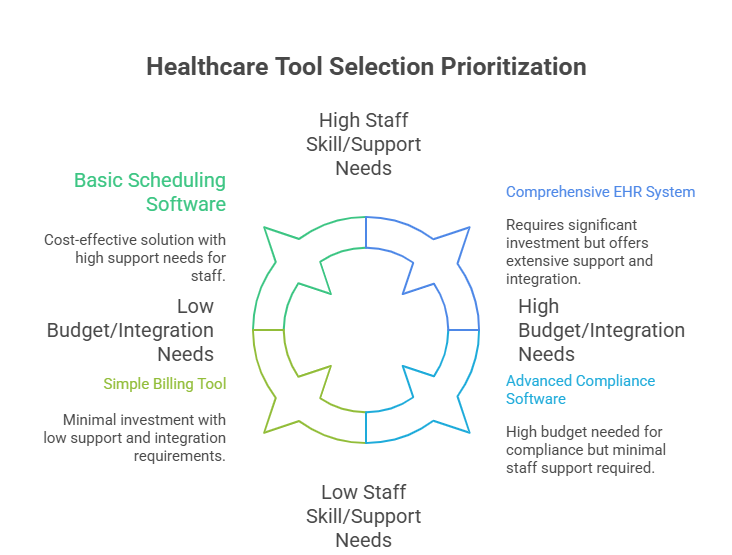
How to Choose the Right Tool for Your Facility
Choosing the right project management software for your healthcare organization isn’t just about features—it’s about fit, compliance, and long-term usability. Below are the most critical factors you must evaluate before committing to a platform.
Budget, Integration Needs, Staff Skill Level
Healthcare budgets are often tightly allocated, and leadership must justify every software investment. Consider not just the license cost but also implementation, training, and support expenses. Many enterprise-grade tools charge extra for HIPAA compliance, which is non-negotiable for most providers.
Integration is equally essential. Your PM tool must plug into EHRs, patient scheduling systems, finance software, or even research databases. If it lacks built-in connectors or open APIs, your IT team will face costly customization and delays. Tools like ClickUp and Smartsheet offer better native integrations and API access than more lightweight platforms.
Staff skill level also determines onboarding success. A visually simple tool like Monday may suit admin teams, while power users may thrive in Smartsheet’s spreadsheet-style interface. Choose a platform that aligns with your team’s digital fluency to avoid adoption bottlenecks and project slowdowns.
Support & Healthcare-Specific Templates
Ongoing support is a critical but often overlooked differentiator. Vendors that provide live onboarding, healthcare-specific walkthroughs, and regional compliance documentation can dramatically improve time-to-productivity. Prioritize platforms that offer dedicated healthcare account reps or compliance consultants—especially if your operations span multiple states or regions with varying laws.
Templates are another time-saver. Tools that include prebuilt boards for clinical research, patient intake, or care coordination eliminate the guesswork. ClickUp, for example, provides ready-to-deploy HIPAA-aligned project templates, while Smartsheet offers trial and IRB coordination modules. Avoid tools that require building workflows from scratch unless your team has the internal capacity and governance approval to do so.
In summary, match your choice to the technical stack, compliance requirements, and team composition of your facility. Even a powerful tool will fail if it lacks contextual relevance or overwhelms your users. Let your facility’s workflow—not just a tool’s marketing—be the guide.
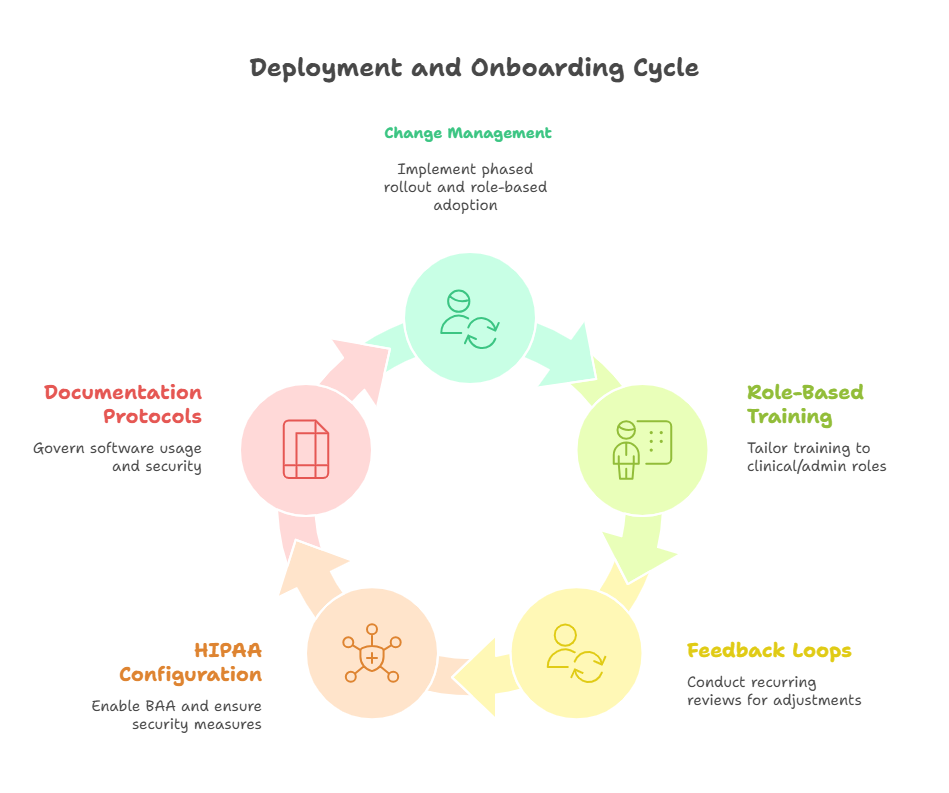
Deployment & Onboarding Best Practices
Rolling out a project management platform in a healthcare environment requires far more than account creation. The stakes are high—delays, non-compliance, or confusion can impact clinical workflows, patient safety, and even billing cycles. Successful deployment relies on careful planning, phased adoption, and robust training.
Change Management, Training, Feedback Loops
Healthcare teams are used to working within tightly regulated structures. Introducing new tools means disrupting established routines, which often leads to initial pushback. Effective change management involves identifying champions in each department, aligning the rollout with compliance milestones, and offering hands-on onboarding. These champions become peer-trainers and internal advocates, making the transition smoother and more credible.
Training should be role-specific. Clinical staff may need guidance on task dependencies, automated reminders, or how to view daily schedules, while finance or IT may focus on integration capabilities or access control. Onboarding isn’t just about walking through features—it’s about showing users exactly how the tool improves their daily responsibilities.
Once deployed, feedback loops are critical. Set up weekly or biweekly check-ins with frontline users to document friction points. Use this feedback to customize dashboards, automate redundant tasks, or refine notification systems. The software should evolve alongside user behavior—not the other way around. Leaders should also monitor adoption metrics, such as active logins, task completions, or overdue actions to identify lagging departments or misaligned processes.
When possible, integrate the PM tool into existing systems. Embedding project updates into EHR dashboards or patient scheduling software ensures workflow continuity without extra logins or redundant data entry.
HIPAA & Compliance Configurations
Even if a platform advertises HIPAA compliance, proper setup is essential. Most platforms require activation of a Business Associate Agreement (BAA) to become compliant. Without it, using the software for PHI (Protected Health Information) may expose your organization to liability—even if the tool supports encryption and access control.
Security configurations must go beyond passwords. Enable multi-factor authentication, define user roles with minimal necessary access, and restrict external file sharing. Tools like ClickUp and Smartsheet allow granular permission settings, including view-only access for auditors or external vendors.
Audit trails should be activated from the start. These logs track every task change, file upload, or user comment—creating a verifiable record for internal QA or external regulatory reviews. Maintain version control policies so that clinical protocols or research tasks reflect the latest approved procedures and prevent accidental reversion to outdated workflows.
Finally, document everything. Your IT, legal, and compliance teams should work together to create a formal SOP that defines how the software is used, updated, and monitored. This ensures sustainable adoption, supports audits, and gives your project managers confidence that the software is as compliant as your clinical protocols.
Metrics to Monitor Post-Implementation
Rolling out a project management tool in healthcare is only half the battle. To ensure it delivers actual value, organizations must monitor quantifiable performance metrics tied to project efficiency, compliance, and patient safety. These indicators help validate ROI, guide workflow adjustments, and prevent operational drift.
Time Tracking, Task Velocity, Quality Measures
Time tracking is more than productivity monitoring—it’s a visibility tool. In clinical environments, knowing how long it takes to complete tasks like intake processing, EMR transitions, or lab scheduling helps optimize team capacity. Most modern tools include native time logging or can integrate with time-tracking apps to collect this data.
Task velocity is another essential metric. It measures how quickly tasks move through the pipeline—from assignment to completion. A decline in velocity may indicate bottlenecks, unclear ownership, or tool confusion. Tracking these trends weekly helps identify where project managers need to intervene or simplify workflows.
Beyond speed, healthcare PMs must monitor quality. Did the right staff complete the task? Was it done on time? Were there revision requests or compliance flags? These quality signals reveal more about system health than speed alone. Tools like ClickUp allow for custom fields and checklists to assess quality indicators per task, ensuring no corners are cut under pressure.
Combining time, velocity, and quality metrics offers a 360-degree view of project health. When triangulated with patient outcomes or audit results, these KPIs become essential to continuous improvement and risk management.
Continuous Optimization
Once metrics are gathered, optimization isn’t optional—it’s strategic. Set up monthly or quarterly review meetings to analyze trends, user feedback, and workflow inefficiencies. Use this data to refine template designs, update automation logic, or reorganize task hierarchies.
For example, if clinical staff frequently miss pre-op documentation deadlines, the fix might involve moving that task earlier in the sequence, assigning a backup, or creating automated flags. If care coordinators delay discharges due to missing approvals, a custom status or approval field may resolve the delay.
Another overlooked factor is notification fatigue. Teams may receive too many updates, leading to ignored tasks or missed escalations. Audit and streamline notification rules regularly to reduce noise while preserving accountability.
Optimization isn’t just backend. Empower users by letting them customize dashboards or saved filters based on their roles. The more ownership they have, the higher the adoption and the greater the long-term success of the tool.
| Metric | Purpose | Implementation Insight |
|---|---|---|
| Time Tracking | Measures how long tasks take to complete in clinical workflows. | Helps optimize resource allocation, identify overloaded teams, and reduce procedural delays. |
| Task Velocity | Tracks how quickly tasks move from assignment to completion. | Reveals process bottlenecks and highlights misalignments in responsibility or tool use. |
| Quality Indicators | Assesses task accuracy, timeliness, and number of revisions or compliance issues. | Ensures procedures meet quality standards without shortcuts or rework. |
| User Adoption Metrics | Monitors tool usage—logins, completion rates, overdue tasks, etc. | Identifies teams that may need additional support, training, or configuration changes. |
| Optimization Triggers | Highlights patterns for improving workflow design and notification settings. | Guides template refinements, automation adjustments, and overall platform ROI. |
Build True Healthcare PM Expertise with APMIC’s Advanced Certification
Even the best project management software can’t deliver results without the right leadership behind it. If you're managing clinical workflows, hospital-wide initiatives, or digital health transformation projects, you need more than tool familiarity—you need strategic, healthcare-specific PM mastery. That’s exactly what APMIC’s Advanced Project Management Certification delivers.
This certification goes far beyond general frameworks like Agile or PMP. It’s built for healthcare professionals who want to lead cross-functional teams, navigate compliance-heavy timelines, and implement enterprise-grade systems like EHRs or RPM platforms. With 542 lessons, case-based simulations, and real-world tool integration modules, learners graduate ready to drive outcomes in clinical, research, and public health settings.
The course includes detailed breakdowns of workflow mapping, resource allocation, regulatory adherence (HIPAA, FDA, IRB), and real-time KPI monitoring—all mapped directly to today’s healthcare tools. Whether you're selecting software, onboarding teams, or reporting to C-suite execs, this certification gives you the frameworks and credibility to lead.
Interested in mastering both the technical and operational demands of healthcare project management? Explore the APMIC Advanced Project Management Certification and take the lead on high-stakes initiatives with confidence.
Frequently Asked Questions
-
Healthcare project management operates in a regulated, high-stakes environment where delays or miscommunication can impact patient safety. Unlike standard industries, it must account for HIPAA compliance, clinical workflows, and multi-disciplinary coordination involving physicians, nurses, administrators, and IT. Timelines are often tied to patient procedures, research deadlines, or compliance audits, which require more than just checklists—they demand audit trails, role-based access, and incident escalation features. The pressure to maintain both operational efficiency and legal compliance makes healthcare project management uniquely complex. As a result, tools must integrate deeply with EHRs, patient databases, and scheduling systems to be truly effective.
-
ClickUp and Smartsheet are top choices for hospital project management due to their customization, compliance support, and cross-functional coordination features. ClickUp offers HIPAA-compliant plans, healthcare templates, and strong automation capabilities that simplify recurring clinical tasks. Smartsheet, on the other hand, provides enterprise-grade dashboards and formula logic suited for multi-departmental coordination. Both platforms support role-based permissions and detailed audit logs—critical for hospital compliance. While Asana and Monday.com offer intuitive UIs, they may lack the depth or healthcare-specific features required by larger facilities. Ultimately, hospitals should prioritize platforms that handle compliance complexity, not just task tracking.
-
While tools like Trello and Notion are useful for simple project tracking, they generally fall short in healthcare environments. They lack built-in HIPAA compliance, audit logging, and structured role-based access—which are essential when dealing with Protected Health Information (PHI) or clinical task workflows. Additionally, they don’t offer healthcare templates or integrations with EHRs, billing systems, or lab scheduling software. Using such tools without compliance safeguards can lead to data exposure and legal violations. If you're working in a clinical, research, or hospital setting, it's safer and smarter to choose a platform designed with healthcare oversight in mind.
-
For clinical environments, focus on tools that offer HIPAA-compliant plans, role-based permissions, and automated alerts tied to critical milestones like medication administration or discharge preparation. You’ll also want detailed task dependencies, real-time dashboards for patient-facing tasks, and integration with systems like EHRs or lab portals. Templates for care coordination, credentialing, or IRB protocol tracking can save months of setup. Additionally, ensure the tool supports encrypted mobile access, as clinical staff often work across departments. Audit trail logging, customizable user roles, and data residency options are non-negotiable for regulated healthcare environments.
-
Implementation timelines vary based on the facility’s size, the tool’s complexity, and how many departments are involved. For small clinics, onboarding can take 2–4 weeks. In contrast, large hospitals or CROs may require 8–12 weeks, especially if integrations with EHRs or billing platforms are involved. During this period, time is spent on compliance configurations, template customization, training sessions, and feedback loops. Change management is key—rushing deployment without internal champions and staged rollouts leads to adoption failure. Most successful implementations follow a phased approach with milestone-based benchmarks for usability and system coverage.
-
Absolutely. Modern platforms like Smartsheet and ClickUp offer prebuilt modules and templates for managing clinical trial workflows, including IRB submissions, site coordination, recruitment tracking, protocol updates, and adverse event logging. These tools support cross-site visibility, task ownership, and escalation chains for trial milestones—crucial for GCP compliance. You can also automate reminders for patient follow-ups, consent form renewals, and lab result entry. Plus, real-time dashboards allow CROs and sponsors to monitor progress across geographies. A well-configured PM tool can drastically reduce delays, improve documentation quality, and enhance collaboration between clinical teams and trial stakeholders.
-
No. HIPAA compliance is not automatically included—even in software that claims to be secure. Compliance requires a signed Business Associate Agreement (BAA) between the healthcare organization and the software vendor. Without this document, using the platform for handling PHI (like patient data, treatment notes, or lab results) could result in violations—even if the software supports encryption. Additionally, compliance features like access logs, permission management, and secure cloud storage must be properly configured by your IT team. Always verify that the vendor supports HIPAA and request documentation before implementation.
-
Yes. Certifications like the APMIC Advanced Project Management Certification can dramatically accelerate both adoption and effectiveness of healthcare PM tools. Trained project managers understand how to structure workflows, align tasks with clinical priorities, and configure tools in a compliant, scalable manner. The course includes real-world simulations that map directly to tools like ClickUp, Smartsheet, and Monday.com. More importantly, it teaches how to build feedback loops, manage resistance, and ensure long-term team buy-in. With certification, you're not just pushing a tool—you’re leading a transformation that aligns operations, compliance, and outcomes.
The Take Away
Healthcare project management isn’t just about task visibility—it’s about protecting patients, optimizing compliance, and improving care delivery at scale. Choosing the right project management software means balancing flexibility with regulation, ease of use with data security, and functionality with integration readiness. Platforms like ClickUp, Smartsheet, Asana, and Monday.com all offer strengths, but your decision must reflect your facility’s clinical workflows, budget, and compliance risk profile.
Success doesn’t stop at selection. Deployment, change management, feedback loops, and continuous KPI tracking are what transform software into a high-impact operational asset. And while tools are important, the biggest ROI often comes from the people implementing them—trained professionals who understand the regulatory and clinical context.
If you're serious about mastering project delivery in a healthcare setting, invest in training that goes beyond task lists. The APMIC Advanced Project Management Certification is designed for clinical leaders, PMs, and healthcare innovators who want to lead large-scale initiatives with confidence.